“What is…?”
Cue the beat.
Click here to answer.
Have a great weekend ;)!
~ Jacqueline
Residents interested in learning more about ophthalmology should check out the Virtual Introductory Summer Course in Ophthalmology (VISCO), which is a free virtual course on Sunday afternoons this summer that aims to provide increased accessibility to high quality ophthalmology teaching. The first session on Sunday June 19, 2022 3-5pm ET is case-based and focuses on common emergency presentations which your residents may encounter in clinical practice.
The course is composed of two parts:
During the course, you will have opportunities to win prizes and learn ophthalmology from incredible teachers.
The content and objectives of this course are based on a curated list of learning objectives endorsed by Canadian Undergraduate Medical Education Leads in Ophthalmology and reference resources from the Association of University Professors in Ophthalmology (AUPO) and the Medical Council of Canada (MCC).
These sessions are also eligible for Royal College Section 2 CME credits.
More information and links to register can be found here.
Background: Dostarlimab is a humanized monoclonal antibody that binds with high affinity to PD-1, resulting in inhibition of binding to PD-L1 and PD-L2. We report interim data from patients with endometrial cancer (EC) participating in a phase I trial of single-agent dostarlimab.
Methods: GARNET, an ongoing, single-arm, open-label, phase I trial of intravenous dostarlimab in advanced solid tumors, is being undertaken at 123 sites. Two cohorts of patients with EC were recruited: those with dMMR/MSI-H disease (cohort A1) and those with proficient/stable (MMRp/MSS) disease (cohort A2). Patients received dostarlimab 500 mg every 3 weeks for 4 cycles, then dostarlimab 1000 mg every 6 weeks until disease progression. The primary endpoints were objective response rate (ORR) and duration of response (DOR) per RECIST V.1.1, as assessed by blinded independent central review.
Results: Screening began on April 10, 2017, and 129 and 161 patients with advanced EC were enrolled in cohorts A1 and A2, respectively. The median follow-up duration was 16.3 months (IQR 9.5–22.1) for cohort A1 and 11.5 months (IQR 11.0–25.1) for cohort A2. In cohort A1, ORR was 43.5% (95% CI 34.0% to 53.4%) with 11 complete responses and 36 partial responses. In cohort A2, ORR was 14.1% (95% CI 9.1% to 20.6%) with three complete responses and 19 partial responses. Median DOR was not reached in either cohort. In the combined cohorts, the majority of treatment-related adverse events (TRAEs) were grade 1–2 (75.5%), most commonly fatigue (17.6%), diarrhea (13.8%), and nausea (13.8%). Grade≥3 TRAEs occurred in 16.6% of patients, and 5.5% discontinued dostarlimab because of TRAEs. No deaths were attributable to dostarlimab.
Conclusion: Dostarlimab demonstrated durable antitumor activity in both dMMR/MSI-H (ORR 43.5%) and MMRp/MSS EC (ORR 14.1%) with a manageable safety profile.
More on Safety and antitumor activity of dostarlimab in patients with advanced or recurrent DNA mismatch repair deficient/microsatellite instability-high (dMMR/MSI-H) or proficient/stable (MMRp/MSS) endometrial cancer: interim results from GARNET—a phase I, single-arm study via Journal for ImmunoTherapy of Cancer.
“Background and Objectives: Transcutaneous electrical stimulation of low- and medium-frequency currents is commonly used in pain management. Interferential current (IFC) therapy, a medium frequency alternating current therapy that reportedly reduces skin impedance, can reach deeper tissues.
IFC therapy can provide several different treatment possibilities by adjusting its parameters (carrier frequency, amplitudemodulated frequency, sweep frequency, sweep mode or swing pattern, type of application (bipolar or quadripolar), time of application and intensity). The objective of this review article is to discuss the literature findings on the analgesic efficacy of IFC therapy.
Conclusions: According to the literature, IFC therapy shows significant analgesic effects in patients with neck pain, low back pain, knee osteoarthritis and post-operative knee pain. Most of the IFC parameters seem not to influence its analgesic effects. We encourage further studies to investigate the mechanism of action of IFC therapy.”
More on Analgesic Effects of Interferential Current Therapy: A Narrative Review via Medicina (Kaunas). 2022 Jan; 58(1): 141.
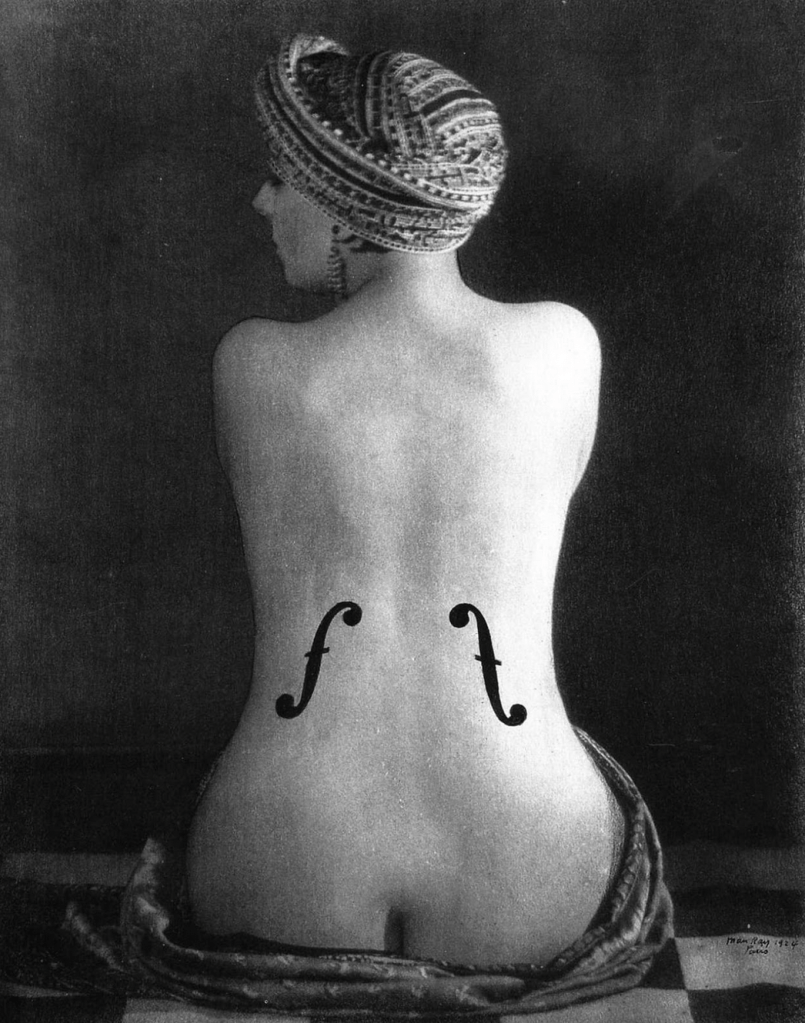
The Body Electric was launched at ICRE 2014. An inspiring selection of visual art, in a range of media – photography, drawing, painting, sculpture and film – explored the conference theme of medical technology from new critical and artistic angles.
This year, The Body Electric jury is looking for visual art submissions on the theme Art as Coping, Art as Community in Healthcare, to reflect the ICRE 2022 theme, Together Again: A Community Redefining Residency Education.
You are invited to approach the theme broadly to consider these themes from various experiential and critical perspectives, such as:
Visual art can be submitted in any medium; but will be represented digitally.
ARTISTS WHOSE WORK IS INCLUDED IN THE BODY ELECTRIC WILL RECEIVE $100.00 FOR EXHIBITING THEIR WORK
Learn more here.
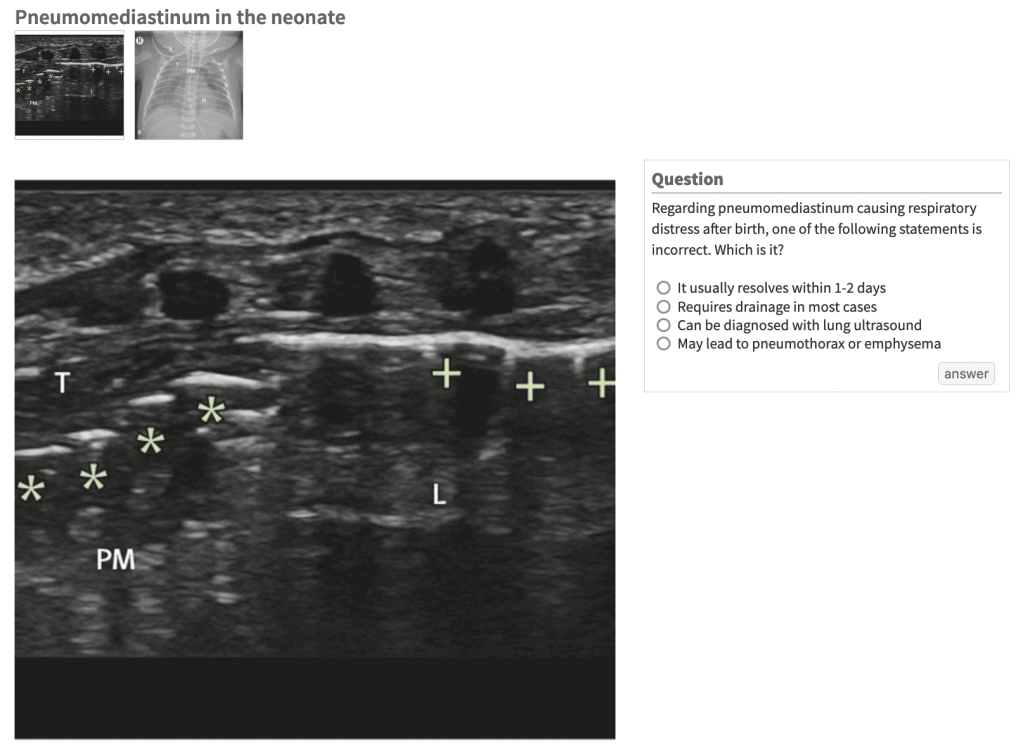
Registration is now open for the newest Rural POCUS Rounds webinar series: Ultrasound for Shock. Over the next six months, we invite you to join us as we discuss five topics specific to the application of ultrasound for shock. Each session will include a presentation on the topic, relevant case studies and a Q&A session.
Jun–Nov 2022 (Fridays) | 1200–1300 PT
Audience: health-care providers working in and supporting rural communities.
Overview: Rural POCUS Rounds is a monthly, interactive Zoom series aimed at providing rural health-care providers with up-to-date and relevant POCUS education. Join us on the last Friday of every month!
Up to 1.0 Mainpro+/MOC Section 1 credits per session
Free — thanks to funding from the JSC
Jun 24 | Dr. Tracy Morton
LEARN MORE & REGISTER
Aug 26 | Dr. Tracy Morton
LEARN MORE & REGISTER
Sep 30 | Dr. Kevin Fairbairn
LEARN MORE & REGISTER
Oct 28 | Dr. Kevin Fairbairn
LEARN MORE & REGISTER
Nov 25 | Dr. Tracy Morton
LEARN MORE & REGISTER

“‘PS,’ an 83-year-old woman, was diagnosed in June 2009 with advanced, metastatic inflammatory breast cancer. At the same time, she began chemo-therapy with Taxol and Herceptin, she also began taking capsules of turkey tail mushroom daily. The dose was 4 g twice daily (Host Defense Turkey Tail capsules, Fungi Perfecti Laboratories, Kamilche Point, Washington). The turkey tail capsules consist of activated, freeze-dried, organic mushroom mycelium, containing polysaccharides (beta-glucans, arabinoxylane, glucose, xylose, galactose, mannose, glycoproteins, ergosterols, triterpenoids, and other myconutrients). In December 2009, when the patient’s chemotherapy regimen was completed and she began Herceptin maintenance therapy every 3 weeks, she continued to take 4 g daily of turkey tail mushrooms and added a combination mushroom formula (Host Defense MyCommunity capsules, Fungi Perfecti, Laboratories). This preparation consisted of 17 species of activated, freeze-dried, organic mushroom mycelium, containing polysaccharides (beta-glucans, arabinoxylane, glucose, xylose, galactose, cordycepic acid, glycoproteins, ergosterols, triterpenoids, and other myconutrients).
Turkey tail mushrooms grow in a woodland environment worldwide and have been reported to stimulate immune function in women with breast cancer. They are called bracket fungi because they form thin structures in concentric circles and grow almost everywhere trees are found. This species of mushrooms has a history of use in Asia as a nonspecific immune modulator, and in breast cancer patients, they have been shown to interact with the CR3 membrane receptors for beta-glucans.1 Immune modulation is believed to be the primary mechanism of action of turkey tail mushrooms.2 The University of Minnesota and Bastyr University (Kenmore, Washington) recently completed a phase 1 dose-escalation trial and found that up to 9 g/day of a T versicolor preparation is safe and tolerable in women with breast cancer who had undergone chemotherapy.3 Perhaps the most intriguing part of this study was the finding that 6 g of T versicolor appeared to lead to faster immune recovery after radiotherapy. This should be studied in additional clinical trials on the potential primary and secondary effects of mushroom therapy in patients with cancer and, more specifically, cancers with altered CR3 membrane receptors.”
Learn more on Trametes versicolor (Turkey Tail Mushrooms) and the Treatment of Breast Cancer via Glob Adv Health Med.

Question Does the addition of metformin to standard breast cancer treatment improve invasive disease–free survival?
Findings This randomized clinical trial included 3649 patients with high-risk operable breast cancer without diabetes. Treatment with metformin vs placebo resulted in a hazard ratio for an invasive disease–free survival event of 1.01; this was not statistically significant.
Meaning Addition of metformin to standard breast cancer treatment did not significantly improve invasive disease–free survival.
Effect of Metformin vs Placebo on Invasive Disease–Free Survival in Patients With Breast Cancer: The MA.32 Randomized Clinical Trial via JAMA.
Hello Residents and Faculty!
Just a reminder that tomorrow we have our curriculum mapping workshop. Dr. Thanh Luu & I will be facilitating the process. Please see the documents linked below that we’ll be referencing throughout the session.
Domains of Care & Core Activities: Core Learning Outcomes (May 2020)
Residency Training Profile for Family Medicine and Enhanced Skills Programs Leading to Certificates of Added Competence via CFPC (May 2021)
See you soon,
Jacqueline
“The first HVIP, Caught in the Crossfire, was launched in 1993 in Oakland, Calif., to offer wraparound mentoring, legal, employment and mental health supports to young people who are in the hospital recovering from a gun injury. Researchers from the University of San Francisco Medical Center evaluated the program and found that participants were 70 percent less likely to be arrested for any offense and 60 percent less likely to be involved in any criminal activity, compared to a control group who did not receive the program’s services. Participants in another gun violence intervention program at the University of Maryland Medical Center were far less likely to be shot again; only 5 percent of those in the program were reinjured, compared to 36 percent who were not in the program.
Over 90 percent of adults who live in homes with guns say they have never discussed firearm safety with a clinician; in an effort to lower that figure, Northwell is conducting a first-of-its-kind National Institutes of Health–funded study. We are currently piloting a universal screening protocol where we ask our patients questions about their exposure to firearms to better understand their risk of being on one end of gun violence or the other.
For the pilot, providers in our health system talk to patients who comes into three of our hospitals about how to avoid gun injuries—the same way we talk to them about sugar intake, exercise, or motor vehicle safety. Previously, there was no standardized procedure for when and how clinicians should have these conversations. We now talk to patients who have access to firearms about safe storage, provide them with gun locks and connect those at risk of gun violence with appropriate intervention services—like peer mentors, mental health support, job training programs, and more.”
Learn more on Gun Violence Is an Epidemic; Health Systems Must Step Up via Scientific American.