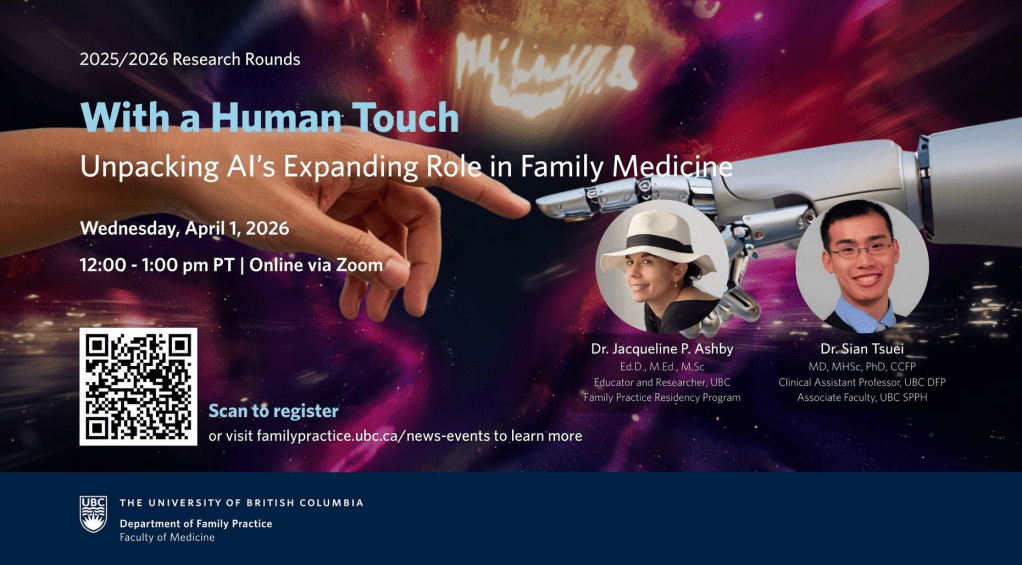
AI’s expansion in the academic and clinical learning environment is raising questions about the role of advanced technologies in education and patient care. This panel explores how primary care clinicians and medical educators are exploring the application of AI, in addition to its tensions, opportunities, and concerns in its current and future use.
The focus of this conversation is to share insights, research, perceptions, and experiences with the use of AI in our academic and healthcare settings.
Learn more and register here: https://familypractice.ubc.ca/april-2026-research-rounds-a-in-family-medicine/
Submit and vote on questions you’d like to see during this Q&A: https://www.questionwave.com/q/ej0Yjkkf79