
To register, please click here.

To register, please click here.
“Imagine that you are on the waiting list for a non-urgent operation. You were seen in the clinic some months ago, but still don’t have a date for the procedure. It is extremely frustrating, but it seems that you will just have to wait.
However, the hospital surgical team has just got in contact via a chatbot. The chatbot asks some screening questions about whether your symptoms have worsened since you were last seen, and whether they are stopping you from sleeping, working, or doing your everyday activities.
Your symptoms are much the same, but part of you wonders if you should answer yes. After all, perhaps that will get you bumped up the list, or at least able to speak to someone. And anyway, it’s not as if this is a real person.
The above situation is based on chatbots already being used in the NHS to identify patients who no longer need to be on a waiting list, or who need to be prioritised.”
Read more on “You could lie to a health chatbot – but it might change how you perceive yourself” via The Conversation.
“From family medicine clinics to specialist units around British Columbia, there are more than 1300 UBC resident doctors training in regional, rural and remote communities.
Guided by UBC clinical faculty, resident doctors provide compassionate care to families and patients, and play a crucial role in our healthcare system. They also contribute their skills and knowledge beyond the clinic.
‘Resident doctors support the education of medical students, conduct research and strengthen health care as they train to become expert practitioners in numerous specialties,’ says Dr. Ravi Sidhu, Associate Dean of Postgraduate Medical Education. ‘I am grateful for their dedication to serving and enhancing health of communities across B.C.’
Thank you to all UBC resident doctors for the care you provide communities across B.C.
As part of Resident Doctors Appreciation Week, we caught up with a few UBC resident doctors to learn more about their experience by asking the following question: ‘How has residency training informed your future practice?’”
Read their responses here.
Health is produced by a complex interplay of individual, social, political, and economic factors. Interdisciplinary and cross-faculty collaborations have the potential to lead to more innovative solutions to improve health and address health inequities.
The Health Innovation Funding Investment (HIFI) Awards are intended to catalyze these collaborations by supporting cross-faculty and cross-campus research at UBC’s Vancouver and Okanagan campuses.
Awards of $10,000 to $25,000 will be granted to faculty members who are collaborating across faculties, disciplines, and campuses to develop new teams, pursue new ideas, or translate findings from innovative health-related research.
Funding projects should align with UBC Health’s strategic priorities and have a direct impact on the health and wellbeing of individuals, communities, and societies.
Next call opens February 2024! Learn more here.
“By 2050, almost one out of every four people who develop dementia in Canada will be of Asian origin, a 785 per cent increase from 2020, says a report released this week by the Alzheimer Society of Canada. The report, based on modelling by the Canadian Centre for Economic Analysis, says the overall number of people living with dementia is projected to rise to one million by 2030, nearly triple the current amount. It focuses on the diversity of people who will be developing dementia as the population ages, and the need for services to be tailored for various racialized groups.”
Read more on Rising dementia rates among Asian Canadians call for culturally safe services: Report via Global News.
Also see Navigating the Path Forward for Dementia in Canada: The Landmark Study Report #1 via Alzheimer Society of Canada.
“Low back pain is a leading cause of disability worldwide, affecting about 570 million people globally. About 39% of the adult population will have low back pain in any given year. Low back pain is costly; in the United States, health care spending on low back pain was $134.5 billion annually between 1996 and 2016 and is increasing. Clinical guidelines recommend triage to identify symptoms that require diagnostic investigation (prevalence of serious pathology < 1% in primary care). Nonspecific low back pain, where no specific pathoanatomical cause can be identified, is the most common type of low back pain. Management focuses on reducing pain and its consequences through education and reassurance, nonpharmacological treatments (e.g., heat, relative rest, staying active), analgesic medicines (e.g., nonsteroidal anti-inflammatory drugs) and timely review.
Existing literature suggests that the clinical course of an episode of low back pain is favourable. However, recurrence is common (about 69% of patients will experience recurrence within 12 months) and pain persists for many patients. Several studies have shown that acute low back pain is not always associated with a favourable outcome, including 2 systematic reviews that showed that, although many patients recover within the first month, low levels of pain and disability often persist.”
Read more on “The clinical course of acute, subacute and persistent low back pain: a systematic review and meta-analysis” via CMAJ.
“As the natural route of infection with tuberculosis is through inhalation of droplets into the lungs, this study, which delivers BCG by the same route, is hoped to be better at stimulating the immune system.
Prof Helen McShane Chief Investigator, TB Vaccine Trials Jenner Institute, University of Oxford, said:
TB kills more people than any other infectious disease and we urgently need better vaccines. This important new study will help us to see whether giving BCG more than once stimulates a stronger immune response and whether giving it by inhalation is better than giving it into the skin. Small studies like these are really important to help us understand the immune response in people and allow us to design and test better vaccines.
This study will also explore whether giving people with Type 2 Diabetes BCG in the skin stimulates as strong an immune response as giving BCG in the skin to healthy people without diabetes. We know that people with type 2 diabetes are more likely to get TB and part of this may be because the BCG vaccine does not work as well in this group.”
Learn more on Novel inhaled TB vaccine via University of Oxford.
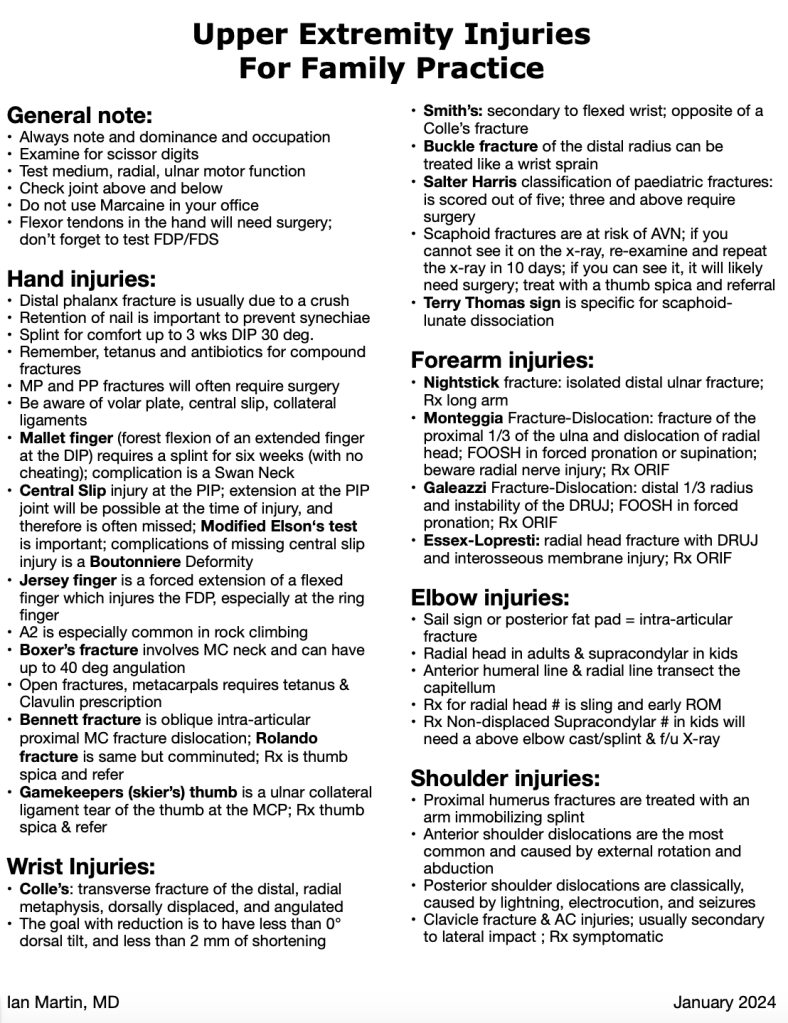
A big thank you to Dr. Ian Martin for his academic half day presentation on “X-Rays: Part I” and for sharing his handout on upper extremity injuries for family practice.
“When I started my medical training in 1984, the general understanding was that clinical history contributed about 70% to establishing a diagnosis, with physical examination and investigations contributing about 20% and 10%, respectively. Since then, remarkable advancements in medical imaging (MRI became widely available only in the early 1990s), other rapidly advancing technologies, practice pressures, and virtual care have all influenced the role of the physical exam.
WorkSafeBC depends on external information to adjudicate a worker’s claim and relies on the information physicians submit to support the worker’s treatment and recovery from a workplace injury or illness. When a WorkSafeBC medical advisor (a physician) reviews claims, they also review the examination findings from attending physicians. Missing or incomplete findings can impact a worker’s entitlement to WorkSafeBC benefits such as physiotherapy and expedited assessments, investigations, and surgery. Missing information also makes it difficult to identify safe options for a graduated return to work, which can imperil a worker’s livelihood.”
More on Perspectives on the value of the clinical exam for your patients with work-related medical conditions via BCMJ.