Last night I attended the “From Hype to Hospital: How AI is being used in Healthcare and Research” hosted in British Columbia, Canada.
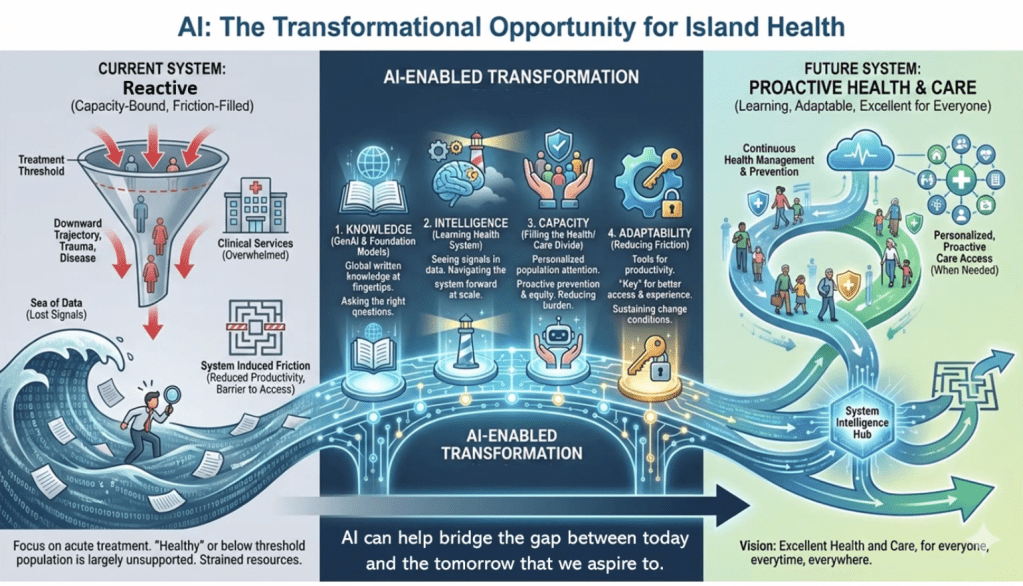
We’re surrounded by data in our healthcare system, but our ability to convert it into timely, trustworthy decisions is still limited by workflow, infrastructure, and governance. Provincial data collection continues to be labour intensive, often manual, and delayed.
As it was reported this evening, in trauma care, there can be a 12-18 month lag between what happens in the Emergency Department and Trauma Service, and what ultimately lands in registries, dashboards, and system-level reports. Check out the article “iROBOT: Implementing Real-time Operational dashBOards for Trauma care” to learn more: https://lnkd.in/gvBQKMgs
Other interesting points from presenters include:
+ Structured data is easy to analyze, narrative data holds the nuance that can change risk and interpretation.
+ AI can speed screening and reporting, reduce false positives, and support real-time dashboards, if evaluated honestly.
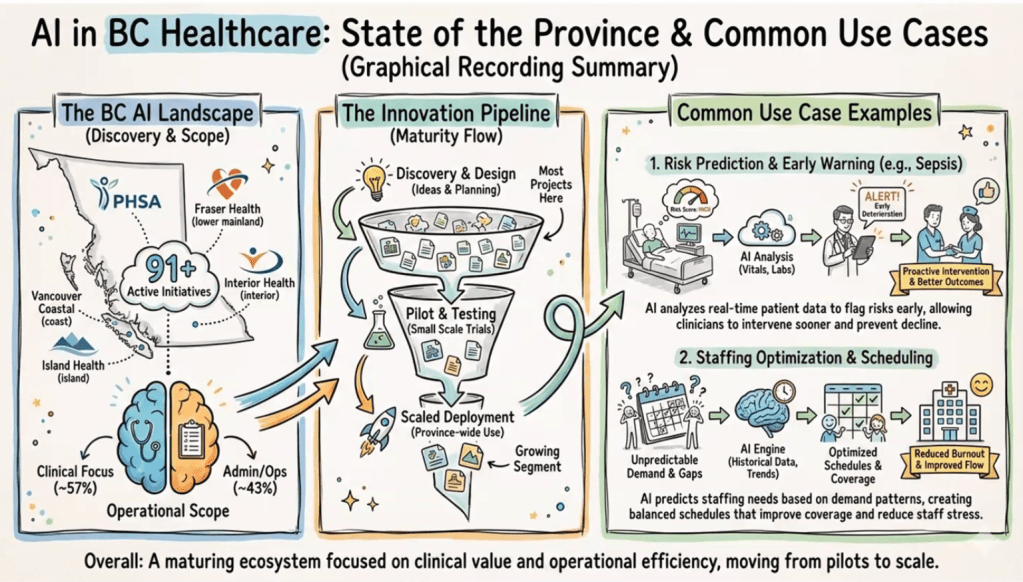
+ In BC, common use cases are emerging: early warning (sepsis, deterioration), staffing and scheduling, operational intelligence.
+ The hard part is the pipeline: discovery to pilot to scaled deployment, many projects stall before impact.
+ Implementation risks are real: trust (confabulation, over-reliance), privacy, environmental cost, workforce disruption.
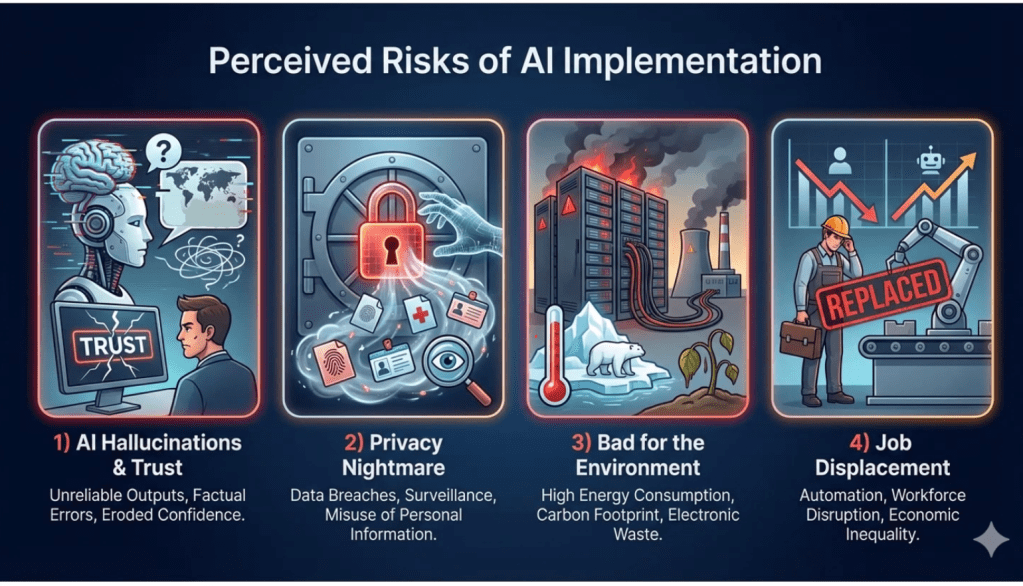
My takeaway: We have a responsibility to educate and train healthcare practitioners in the use of AI, and to start asking critical questions about how it will affect patient care.
Slides attached are from Graham Payette’s AI BC briefing.
Sincerely,
Jacqueline
